When a dental implant fails, who is to blame? This question is debated by dental experts, patients, and insurance companies. Dental implants have a success rate of 96.4% over 10 years. Yet, the small failure rate still impacts thousands yearly.
A recent survey by Nitzan Levy found interesting results. Who is responsible for dental implant failures The survey showed 53% of dental professionals blame dentists. Only 13% blame patients. Just 5% say it’s the implant’s fault, and 28% point to biological factors.
Success with dental implants depends on many factors. The dentist’s skill, the patient’s health, and the implant quality are all important. Early failures often happen before the implant is used, due to bone issues or surgical problems. Late failures occur when the implant is used, usually from mechanical issues or infections like peri-implantitis.
Figuring out who is to blame for dental implant failures needs a close look at each case. The shared responsibility model says success comes from teamwork. It requires skilled dentists, committed patients, and reliable implants.
Key Takeaways
- Dental implants succeed in 96.4% of cases over 10 years
- Most dental professionals (53%) believe dentists bear primary responsibility for failures
- Early failures occur before loading due to integration problems
- Late failures happen after loading from mechanical or infectious causes
- Success requires cooperation between dentist, patient, and quality implant systems
- Only 5% of professionals blame the implants themselves for failures
- Biological factors account for 28% of unpredictable failures
Understanding Dental Implant Success and Failure Rates
Modern dentistry has made a big leap in tooth replacement. Dental implant success rates are very high, with 96.4% still working after 10 years. This shows how far we’ve come in making these implants better for millions of people every year.
Current Statistics on Implant Survival
Recent implant survival statistics look very good for those thinking about getting implants. Studies say 90-95% of implants work well for 15 years or more if done right. Dental implants have about 97% success over 10 years, making them a top choice for fixing teeth.

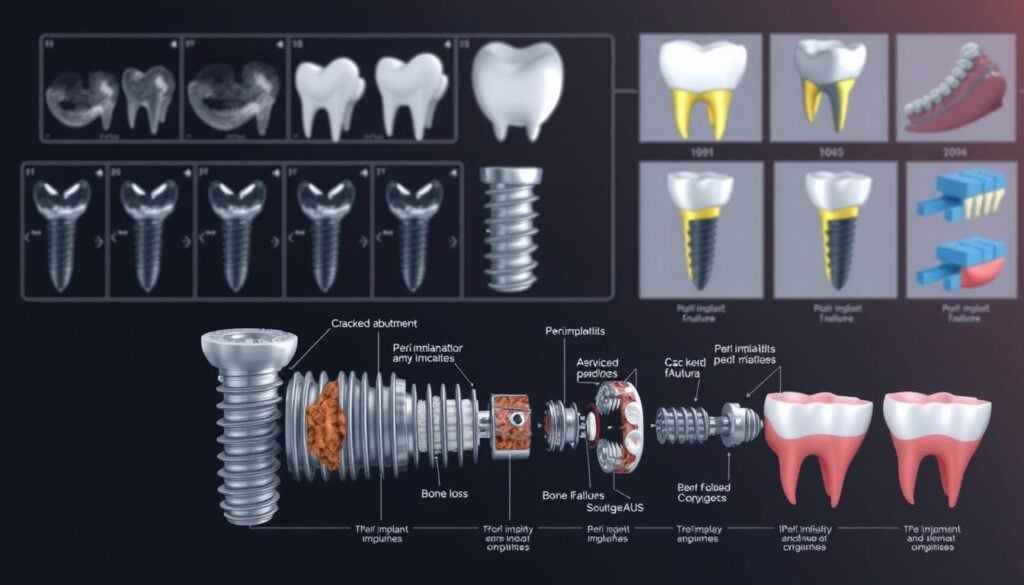
Early vs. Late Implant Failures
Knowing about early vs late implant failure helps patients understand possible problems. Early failures happen before the implant is used for chewing, usually in the first few months. Issues like bad bone healing, surgery problems, or infection can cause these early failures.
Late failures happen after the implant is used for chewing, sometimes years later. Problems like gum disease around the implant or too much pressure from biting can lead to these failures.
Industry Benchmarks and Expected Outcomes
Professional standards set clear goals for how well treatments should work. Top implant makers and dental groups keep a close eye on results. These standards help doctors aim for the best results by following proven methods and choosing the right patients.
The Complex Nature of Implant Failures
Dental implant failures often come from many problems working together. Factors leading to implant failure are complex. This complexity helps patients and dentists work together to prevent issues.
Research shows that implant failures fall into three main categories:
- Patient-related factors – Including overall health, bone quality, and lifestyle choices
- Surgical and prosthetic factors – Covering placement techniques and restoration design
- Implant-specific factors – Such as material quality and surface characteristics
When looking at complex implant failure causes, dental professionals see that focusing on one thing is not enough. A patient with diabetes might heal slower. But, if the surgeon uses excellent technique and the patient keeps good oral hygiene, the implant can still succeed.
Even the best implant can fail if many risk factors come together.
“Success in implant dentistry requires attention to every detail, from initial planning through long-term maintenance. No single factor guarantees success or failure.”
This complex nature of implant complications means prevention needs a team effort. Dentists must look at all risk factors during planning. Patients also need to understand their part in keeping the implant healthy. Recognizing these complex implant failure causes early helps in better treatment planning and more reliable results.
Patient-Related Factors in Implant Failure
Dental professionals are key to implant success. But, patient-specific traits often decide if an implant will succeed or fail. Knowing these traits helps both doctors and patients understand what to expect and how to prevent failures. Studies reveal that health status, daily habits, and biological differences greatly affect implant success.
Systemic Health Conditions
Some medical conditions are major causes of implant failure. Diabetes, especially if not well-managed, hinders healing. People with diabetes over 200 mg/dL are at higher risk of implant problems than those without diabetes.
Osteoporosis is another issue. It weakens bones, making it hard to place implants securely. The International Team for Implantology says patients with severe osteoporosis might need special treatments or bone grafts before surgery.
Lifestyle Factors and Habits
Smoking is a big risk for implant failure. Nicotine cuts off blood flow to healing areas, increasing failure rates by up to 140%. Past gum disease is also a worry, as it can lead to new infections around implants.

Oral Hygiene and Maintenance
Bad oral care habits let bacteria grow. Brushing, flossing, and regular dental visits are crucial. Skipping these can increase the risk of implant problems by 25% in five years.
Bone Quality and Quantity
Good bone structure is vital for implant success. Thin or soft bone can’t hold implants, leading to failure. Dentists use advanced imaging to check bone density before surgery. This helps identify who might need extra bone procedures.
Surgical and Technical Factors
Your dental surgeon’s skill is key to implant success. Surgical complications in dental implants can happen if the procedure isn’t done right. Knowing these factors helps patients and doctors work together to lower risks.
Implant Placement Precision
Getting the implant in the right spot is crucial. Technical issues often come from wrong placement. The surgeon must think about bone density, space, and how close it is to nerves and sinuses.

Heat Generation and Surgical Trauma
Drilling into bone can hurt the tissue around it. Skilled surgeons use irrigation techniques and slow drilling to avoid overheating. The implant placement procedure needs careful handling to help healing and bone integration.
Three-Dimensional Positioning
Modern implant surgery needs precise 3D positioning for success. The implant must be placed correctly:
- At the right depth for crown emergence
- At the correct angle for force distribution
- Far enough from other teeth
- In the right spot in the bone
Advanced imaging and surgical guides help get the implant in the best spot. This reduces complications and improves results.
Who Is Responsible for Dental Implant Failure
Patients often ask who is to blame when dental implants fail. The truth is, success in dental implants comes from teamwork. Surveys show different views on who is at fault for dental implant failure.
Shared Responsibility Model
Success in dental implants needs the dentist, patient, and implant maker to work together. The dentist must diagnose correctly, place the implant accurately, and follow up. Patients must keep their teeth clean, go to all appointments, and manage health issues. The maker of the implant must ensure it’s of high quality.
Professional Perspectives from Recent Surveys
A LinkedIn survey shed light on dental professionals’ views on dental implant failure responsibility. The results show a mix of opinions:
| Responsibility Attribution | Percentage of Respondents | Key Contributing Factors |
|---|---|---|
| Dentist/Surgeon | 53% | Poor technique, inadequate planning, surgical errors |
| Unpredictable Factors | 28% | Biological response, unforeseen complications |
| Patient | 13% | Poor hygiene, non-compliance, smoking |
| Implant System | 5% | Material defects, design flaws |
Legal and Ethical Considerations
Knowing who is responsible for dental implant failure is key when problems happen. Legal cases often look at if the dentist followed the right steps, like getting consent and doing the right tests. Dentists should know their limits and send hard cases to specialists. Keeping good records is important to figure out if the dentist did everything right.
The Role of Pre-Existing Medical Conditions
Your health is key to the success of dental implants. A detailed health check is done before surgery. It looks for medical conditions affecting dental implants that could harm the healing or stability of the implant.
Some health problems raise the risk of pre-existing conditions implant failure. High blood sugar from diabetes can slow healing and weaken the immune system. Osteoporosis makes it hard for the implant to stay stable in the jaw because of low bone density.
Cancer patients, especially those who got radiation in the head and neck, face higher failure rates. Radiation harms bone cells and blood vessels, making jaw healing hard after implant placement. Autoimmune diseases like rheumatoid arthritis and lupus also hinder healing, making successful implant integration hard.
| Medical Condition | Impact on Implant Success | Failure Risk Level |
|---|---|---|
| Uncontrolled Diabetes | Impaired healing, infection risk | High |
| Osteoporosis | Poor bone density, weak integration | Moderate to High |
| Head/Neck Radiation | Damaged bone cells, poor blood flow | Very High |
| Autoimmune Diseases | Disrupted healing process | Moderate |
Medicines for osteoporosis, like bisphosphonates, can cause problems by messing with bone remodeling. Your eligibility for dental implants depends on these factors. Working with your dentist and doctor is crucial to manage any health issues before surgery.
Impact of Smoking on Implant Success
Smoking is a big problem for dental implants. Studies show smokers are more likely to face implant issues than non-smokers. The harm from smoking and dental implant failure comes from how it affects healing.
Vascular Changes and Healing Impairment
Cigarette smoke harms blood vessels. It reduces oxygen and nutrients to healing areas. This is bad for dental implants because it affects bone growth.
Increased Risk of Peri-Implantitis
Smokers are more likely to get peri-implantitis. This is an inflammation around dental implants. It’s caused by bacteria that thrive in smokers’ mouths.
Statistical Evidence from Recent Studies
Recent studies show smoking’s impact on implants:
- Smokers face a 15.8% chance of implant failure, compared to 6.5% for non-smokers.
- Heavy smokers (more than 10 cigarettes daily) have failure rates near 30%.
- Bone loss around implants is 35% faster in smokers in the first year.
Prosthetic Design and Occlusal Factors
The crown above your gums is key to implant health. Poor crown design can lead to implant problems. It causes stress that damages bone and soft tissues around the implant.
Your bite force is like water pressure in a hose. A good crown spreads pressure evenly. Studies show that how forces hit the implant affects its health. If the crown doesn’t fit right, it can lead to bone loss.
- Crown emergence profile – How the crown emerges from your gums affects cleaning ability and tissue health
- Crown-to-implant ratio – Taller crowns create more leverage and stress on the implant
- Platform switching – Using smaller abutments can redistribute forces more favorably
- Occlusal table width – Narrower chewing surfaces reduce lateral forces
Grinding teeth adds extra stress. Forces from bruxism are much stronger than regular chewing. This can harm implants over time. Wearing night guards is crucial for protection.
Problems from occlusal factors often start slowly. Regular dental visits help catch issues early. Your dentist can spot signs like loose crowns or unusual wear before damage gets worse.
Implant Quality and Manufacturing Standards
The quality of a dental implant is key to success. Not all implants are the same. Knowing the differences in materials, how they’re made, and who checks them helps everyone make better choices.
Material Selection and Surface Characteristics
Titanium is the top choice for implants because it’s safe and strong. Today, implant manufacturing factors focus on making the surface right for bone to attach. Studies show that a certain roughness helps bone attach faster and stronger.
There are special treatments like sandblasting and acid etching to make the surface better. These treatments help bone cells stick to the implant. Top makers spend a lot on these methods to meet high dental implant quality standards.
FDA Approval and Quality Control
In the U.S., implants need FDA approval before they can be sold. This means they pass many tests for safety and how well they work. Famous brands like Nobel Biocare and Zimmer Biomet follow strict rules and get ISO certifications.
| Quality Standard | Requirement | Impact on Success |
|---|---|---|
| FDA 510(k) Clearance | Safety and effectiveness testing | Ensures basic safety standards |
| ISO 13485 | Medical device quality management | Consistent manufacturing quality |
| ASTM F67 | Titanium purity specifications | Optimal biocompatibility |
Counterfeit Implants and Low-Quality Materials
Unfortunately, fake dental implants are out there. They might use bad titanium or skip important steps like cleaning. Look out for very cheap prices, no papers, and no lot numbers.
“Patients should always ask their dentist about the implant brand and request documentation. Legitimate implants come with tracking cards and certificates of authenticity.”
Bad implants can cause allergies, not attach to bone, or break easily. Choosing implants that meet dental implant quality standards lowers these risks and boosts success.
The Importance of Treatment Planning
Good dental implant treatment planning is key to long-term success. New technologies and methods have changed how dentists work with patients. These advancements help lower risks and boost success rates for those getting implants.
Diagnostic Imaging and CBCT Technology
Cone Beam Computed Tomography (CBCT) is now the top choice for dental implant treatment planning. It shows bone structure, nerve locations, and other important details in 3D. Unlike regular X-rays, CBCT scans give a clear view of bone density and volume. This helps dentists spot potential problems before surgery.
Digital Planning Tools
Virtual planning software helps place implants with great accuracy through computer-guided surgery. These tools let dentists:
- Simulate implant placement in 3D models
- Calculate the best angles and depths
- Design guides for precise surgery
- See how the final crown will look before surgery
It’s important to keep 3mm space between implants and 1.5mm from teeth. These exact measurements help avoid preventing implant complications.
Risk Assessment Protocols
Thorough checks help find patients who need special care. Factors that need extra attention include:
| Risk Category | Assessment Focus | Planning Modifications |
|---|---|---|
| Medical History | Diabetes, osteoporosis, medications | Extended healing periods, bone grafting |
| Bone Quality | Density measurements, volume analysis | Alternative implant sizes, augmentation procedures |
| Lifestyle Factors | Smoking status, oral hygiene habits | Cessation programs, enhanced maintenance protocols |
Post-Operative Care and Patient Compliance
Dental implants need more than just the surgery. Patients must focus on post-operative care to ensure healing and stability. Following care instructions is key to successful implant integration with the jawbone.
Success in implant care comes from daily routines. Brush your teeth twice a day with a soft brush, and floss once daily around the implant. Using chlorhexidine mouthwash for the first two weeks can lower infection rates by up to 8.7%.
- Applying ice packs to reduce swelling
- Avoiding smoking and alcohol consumption
- Maintaining a soft food diet initially
- Taking prescribed medications as directed
- Attending all scheduled follow-up appointments
Watch for warning signs. Pain lasting more than 10 days may mean a problem. Early action can stop small issues from becoming big problems. Regular dental cleanings keep the area healthy.
| Time Period | Required Care | Compliance Impact |
|---|---|---|
| First 24 hours | Ice application, rest | Reduces swelling by 60% |
| First 2 weeks | Chlorhexidine rinse | Lowers infection risk by 8.7% |
| Long-term | Daily brushing/flossing | 95% survival rate at 10 years |
Ignoring oral hygiene can lead to implant failure. Skipping dental visits or not cleaning daily increases failure risks. Your effort in post-operative care is crucial for long-term success.
Warning Signs of Implant Complications
Spotting signs of dental implant failure early can save your implant. Your body sends signals when something’s wrong. Paying attention to these implant complication symptoms helps you get treatment before damage gets worse.
Clinical Indicators of Early Failure
Several signs point to implant problems. A loose implant feeling means it’s not fixed right. Trouble chewing or biting might mean it’s not aligned or could hurt nerves. Pain lasting more than 10 days after surgery is a red flag for your dentist.
Gum inflammation, bleeding, or recession around the implant is a sign of infection. Facial swelling that lasts more than 72 hours after surgery is also a warning. Bad breath, pus, or gaps in your smile are serious signs that need quick action.
Radiographic Evidence
X-rays show problems not seen in regular exams. Failed implants have a dark halo on X-rays. Successful ones have white bone around them, showing they’re integrated well. Your dentist uses these to check for bone loss and implant stability before symptoms show.
Patient-Reported Symptoms
Research shows patient feedback is key in spotting complications. Common symptoms include:
- Persistent toothache or throbbing pain
- Metallic taste in the mouth
- Sensitivity to hot or cold temperatures
- Clicking sounds when chewing
- Feeling of pressure around the implant site
| Symptom Type | Timeframe | Action Required |
|---|---|---|
| Mild discomfort | First 3-5 days | Monitor, use prescribed pain relief |
| Severe pain | After 7 days | Contact dentist immediately |
| Bleeding gums | Any time | Schedule appointment within 48 hours |
| Loose implant | Any time | Emergency dental visit |
Legal Recourse and Compensation Options
If dental implants fail due to a dentist’s mistake, you have rights. You can seek compensation for medical costs, pain, and more. Knowing your legal options implant complications is key to getting the help you need.
To win a dental implant failure lawsuit, you must show your dentist was negligent. This involves several steps:
- Gathering all medical records and treatment plans
- Getting high-quality x-rays (not just any images)
- Finding expert dental opinions
- Showing how the dentist’s mistake caused the implant to fail
Reasons for dental implant failure lawsuits include wrong placement, not checking the area well enough, harming nearby tissues, and not fully explaining risks. It’s important for dentists to clearly explain what will happen, the risks, and other options before starting.
| Type of Damages | Typical Compensation Range | Documentation Needed |
|---|---|---|
| Medical Expenses | $5,000 – $50,000 | Bills, receipts, treatment records |
| Lost Wages | $2,000 – $15,000 | Employment verification, pay stubs |
| Pain and Suffering | $10,000 – $100,000 | Medical reports, personal testimony |
| Future Dental Care | $8,000 – $40,000 | Expert projections, treatment plans |
Before suing, check if your surgeon is qualified. Many legal options implant complications cases involve untrained or overmatched dentists. Getting a second opinion can help your case and provide important evidence.
Prevention Strategies for Long-Term Success
Preventing dental implant problems starts before surgery and lasts a lifetime. A good plan combines expert care, patient effort, and regular check-ups. Both dentists and patients must work together to avoid failure.
Evidence-Based Clinical Protocols
Implant success depends on proven methods. Dentists use certain rules for choosing patients, performing surgery, and loading implants. These rules include:
- Complete medical history evaluation
- 3D imaging for precise placement planning
- Sterile surgical environment maintenance
- Appropriate healing time before restoration
Patient Education and Communication
Good communication is key for patient success. Dental teams should teach patients about daily care, diet during healing, and long-term upkeep. Written and visual aids help make this information clear.
Regular Monitoring and Maintenance
Regular visits and cleanings prevent problems. The usual schedule is:
| Time Period | Maintenance Activity | Frequency |
|---|---|---|
| First Year | Professional cleaning and examination | Every 3 months |
| After First Year | Routine maintenance visits | Every 6 months |
| Annually | X-rays and comprehensive evaluation | Once per year |
Catching peri-implant inflammation or bone changes early helps a lot. It leads to better long-term results.
Future Innovations in Implant Technology
The field of dental implants is growing fast. Researchers and makers are coming up with new ways to make implants work better. These new ideas aim to make dental implants more reliable and successful for everyone.
Advanced Biomaterials
Scientists are working on new materials that work well with your body. They’re making titanium alloys that help implants attach to bone faster. Also, new ceramics are being made that are safe for your body and fight off infections.
They’ve also found ways to make implants that help your bone grow around them. Dental experts are using these new technologies to help patients get better results. Even nanotechnology is being used to make implants that feel more like real bone, helping them fit in better.
Digital Workflow Integration
Digital tools are changing how implants are made and placed. Computers help dentists make custom implants that fit each patient perfectly. 3D printing makes guides that help place implants exactly right, cutting down on mistakes.
Virtual reality lets dentists plan the whole procedure before starting. It’s like a practice run. And, new systems guide surgeons during the actual placement, making it safer and more precise.
Conclusion
Dental implant failure is not just one thing. It’s a mix of many factors. Studies show implants work well for most people, but sometimes they fail. It’s not just one person’s fault.
The team, the patient, and the implant all play a part. Proper diagnosis and planning are key. A study on dental implant failures found that 53% of failures are due to the dentist. But, 28% are just unpredictable. Things like smoking and diabetes also matter.
Even top implants can fail if not done right. Success in dental implants needs a team effort. Dentists must use the latest tech and follow proven methods.
Patients should manage their health and keep their mouth clean. Regular check-ups help catch issues early. When everyone does their part, success is more common. This shows that with teamwork, long-term success is achievable.
